Q&A: Rong Fan on “senescent” cells and Yale’s new Tissue Mapping Center
Yale’s tissue mapping center is one of eight supported by NIH’s Cellular Senescence Network (SenNet), a new initiative of the NIH Common Fund program. It will benefit from a $6.5 million grant over five years. Professor Fan discusses what senescent cells are, why they’re important, and how deeper knowledge of them could treat or slow the progression of certain chronic diseases.
Q&A: Rong Fan on “senescent” cells and Yale’s new Tissue Mapping Center
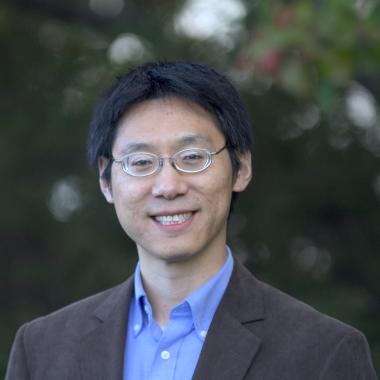
Fan, a professor of biomedical engineering and of pathology, will lead the new Yale Tissue Mapping Center (TMC) for Cellular Senescence in Lymphoid Organs. It’s part of a broad National Institutes of Health-funded consortium aiming to comprehensively identify and characterize differences in senescent cells, which play roles in normal biological processes and also in chronic diseases of aging such as cancer and neurodegeneration.
Fan and a team of Yale investigators will focus on building the first complete catalog of senescent cells in human lymph tissues and on mapping how those cells affect their local environments and tissue functions.
Yale’s tissue mapping center is one of eight supported by NIH’s Cellular Senescence Network (SenNet), a new initiative of the NIH Common Fund program. It will benefit from a $6.5 million grant over five years.
Here, Fan discusses what senescent cells are, why they’re important, and how deeper knowledge of them could treat or slow the progression of certain chronic diseases.
The project focuses on senescent cells. What are those?
They are cells that no longer proliferate, but are still alive. When cells become senescent, some of those are actually very helpful and are physiologically important. For example, some senescent cells produce angiogenic factors that can accelerate the growth of blood vessels and help heal a wound.
On the other hand, we know that when we age, we accumulate more senescent cells, and some may produce the factors that predispose certain types of tissue to a much higher risk of chronic diseases — cardiovascular disorders, pulmonary fibrosis, and things like that.
Senescence in itself is a mechanism for the cells to prevent themselves from developing cancer, because if something is going out of control, the cells become senescent so they can’t grow anymore — that’s actually a defense mechanism. But it’s well known that when those senescent cells accumulate, they create an inflammatory microenvironment, and an inflammatory microenvironment can drive and develop many diseases, including cancer.
Cells that no longer divide — so-called senescent cells — serve human health in certain ways and undermine it in others. Rong Fan of Yale’s School of Engineering & Applied Science and the Yale Cancer Center will assume a major role in a national effort to understand how.
And how is the consortium studying them?
The overarching goal of the consortium is to explore a question regarding what the different types of senescent cells are in human bodies that are important across all biomedical fields — not just cancer or cardiovascular disease, but in all of these different diseases, as well as in aging. The NIH’s Office of Strategic Coordination (OSC) put together this big Common Fund consortium to study them. What is equally important is the tissue context of cellular senescence — where those cells are in that tissue and what impact they generate on other cells in the microenvironment. In our program at Yale, we analyze at the single-cell level the heterogeneity of senescent cells in human lymphoid organs, but we are also doing an analysis of those cells directly in the tissue section.
To do this, we’re using a suite of spatial omics techniques — that is, a study of biological molecules that form and guide organisms, along with their locations within the tissue. To achieve this goal, we assembled a team of investigators at Yale, including clinicians, a pathologist, an immunologist, and a computational biologist to form a Tissue Mapping Center (TMC) to build the first complete catalog of senescent cells in human lymph tissues. But we will also map out how those senescent cells impact their local environments and tissue functions.
Our center is focusing on lymph nodes. Once the cells there become senescent, they’re going to produce many factors that can mess up the normal cell function. And the immune cells may become senescent as well, and then leave the lymphoid tissue and travel through blood circulation to every part of the body. Senescent cells developing in the lymph organs might have a systemic effect, affecting all different organs. We try to map those cells in the lymph organs first, but we also propose to map those in blood so we can identify those senescent immune cells and begin to assess their systemic impact on different physiological systems.
Once you have your tissue maps, what will you do with them?
We will eventually integrate all that data together to build a whole book of different tissue maps — an atlas of tissue maps — across the lifespan and healthspan. Then we can begin to understand how senescent cells develop over different lifespans and health spans.
Ultimately, what could this information lead to?
It could have a significant impact on public health.
At this stage, we need to generate that database so that we know what kind of senescent cells are there and how they impact the tissue microenvironment and function. Maybe some of these senescent cells are valuable because they help the tissue recover from injury, while other senescent cells are really driving the aging process. How do you differentiate that? If you have that knowledge, maybe you can separate the good from bad senescent cells and target the bad ones to slow down aging — especially aging that’s associated with human diseases.
We know lots of chronic diseases are associated with aging, and the senescent cells are shown to be implicated in the development or progression of those diseases. If you can identify the early signs in those bad senescent cells, maybe we can target those cells early on, either to treat or to slow down the progression of chronic diseases, like cardiovascular disease and diabetes.
Departments: Biomedical Engineering